Supporting non-clinical immunotherapy drug development for HCC; new utilization of STAM HCC model
We would like to introduce the features of the STAMTM-HCC/IO+ model as a liver cancer model.
For your reference, we hope you will also visit our special website at the URL below.
https://www.smccro-lab.com/Immuno-oncology/en/
Liver cancer, primarily HCC, is the fourth most common cancer in the world (Huang DQ et al, Nature Reviews Gastroenterology & Hepatology, 18, 223-238, 2021). In particular, the proportion of non-B, non-C HCCs that are not associated with viral hepatitis, such as MASH/NASH, is increasing year by year. In addition to molecular target drugs such as Lenvatinib and Sorafenib, immune checkpoint inhibitors such as Atezolizumab + Bevacizumab, Nivolumab, and Pembrolizumab have recently been used in clinical practice as therapeutic drugs for HCC (Chen C et al, frontiers in Immunology, 14, 1133308, 2023). However, the response rate of immune checkpoint inhibitors for HCC is 0-14%, which is lower than that for other cancers (e.g., melanoma response rate; 35-70%), so there are high expectations for the development of new therapeutic agents (Tan S et al, JACC: CardioOncology, 4, 579-597, 2022, Valero C et al, JAMA Oncology, 7, 1245-1246, 2021).
STAMTM-HCC/IO+ model have the following advantages in tumor immunology:
- It can evaluate the number and localization of infiltrating cytotoxic T cells (CD8-positive T cells).
- It can evaluate the anti-tumor effects by immune checkpoint inhibitors.
- It can evaluate the assessment of tumor growth inhibition by calculating the maximum change rate in tumor diameter of the multiple target lesions by CT.
- The tumor has high tumor mutation burden (Tumor Mutation Burden).
- It can evaluate the tumor microenvironment and its contributing factors (immunosuppressive cells, immune-regulating cytokines/signal transduction, metabolic abnormalities, and gut microbiota). This is because in spontaneously developed HCC, a tumor microenvironment with fibroblasts and immune cells are present, creating an immunosuppressive tumor microenvironment.
We will highlight the actual implementation of immune checkpoint inhibitors (anti-PD-L1 antibodies) and stroma-modifying drugs (TGF-beta neutralizing antibody) using STAMTM-HCC/IO+ HCC model. We hope that these examples will be useful when you consider in-vivo study using STAMTM-HCC/IO+ model.
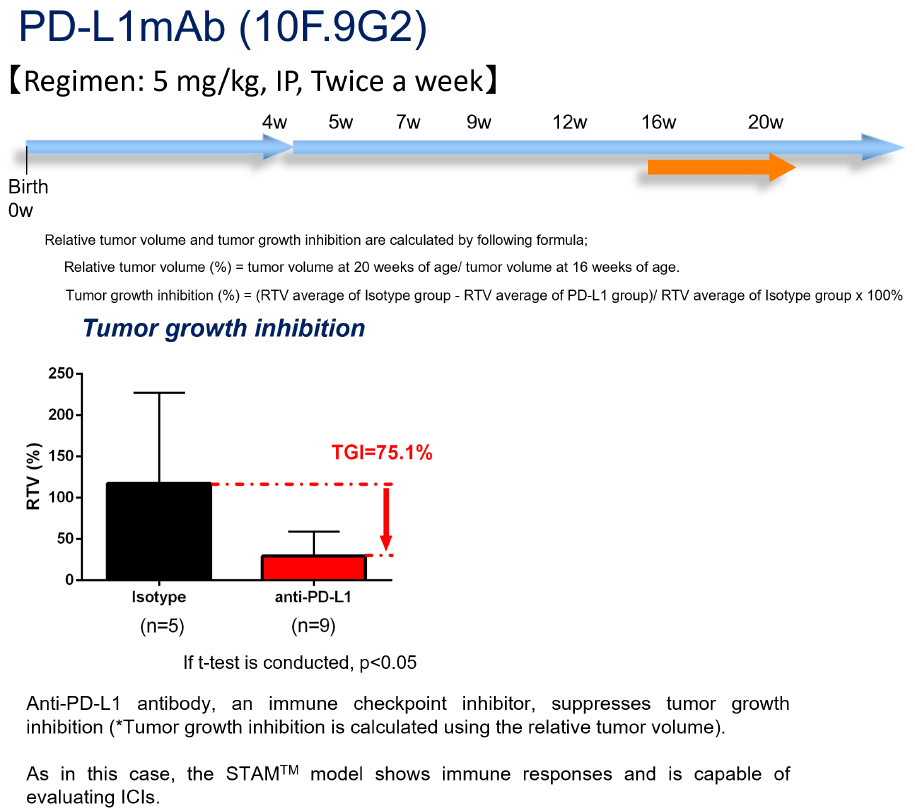
1. Immune checkpoint inhibitors
The anti-PD-L1 antibody (clone; 10F.9G2, clinically used) showed a tumor growth inhibition rate of 75.1% in a HCC treatment study using STAMTM HCC model. It has shown tumor shrinkage effects.
2. Stroma-modifying drugs
The therapeutic effect on HCC has been reported by Okrah et al of Genentech, that the administration of TGF-beta neutralizing antibody (1D11 antibody) improved fibrosis around the tumor and promoted the infiltration of CD8+ T cells into the tumor. (Okrah K et al, NPJ Precision Oncology, 2, 25, 2018).
It has been reported that he efficacy of immune checkpoint inhibitors that are currently used in clinical practice is highly dependent on the tumor microenvironment. Therapeutic targeting of the immunosuppressive tumor microenvironment is thought to provide a new breakthrough in HCC therapeutics (Chen C et al, frontiers in Immunology, 14, 1133308, 2023).
Thus, the STAMTM-HCC/IO+ model is currently the only model that can evaluate the effects of stroma-modifying drugs, which modify the tumor microenvironment in tumors as well as immunotherapy such as immune checkpoint inhibitors.
Would you be interested in non-clinical efficacy evaluation with STAMTM-HCC/IO+ model for HCC therapeutics? In addition to the evaluation of the new drugs, we can evaluate the anti-tumor effects of various immune checkpoint inhibitors, including anti-PD-1 antibodies, in monotherapy studies, as well as in combination studies, and directly compare their anti-tumor effects with those of the anti-PD-L1 antibodies currently used in clinical practice as a control.